Nearly 1 million people in the United States live with multiple sclerosis, a chronic autoimmune disease.
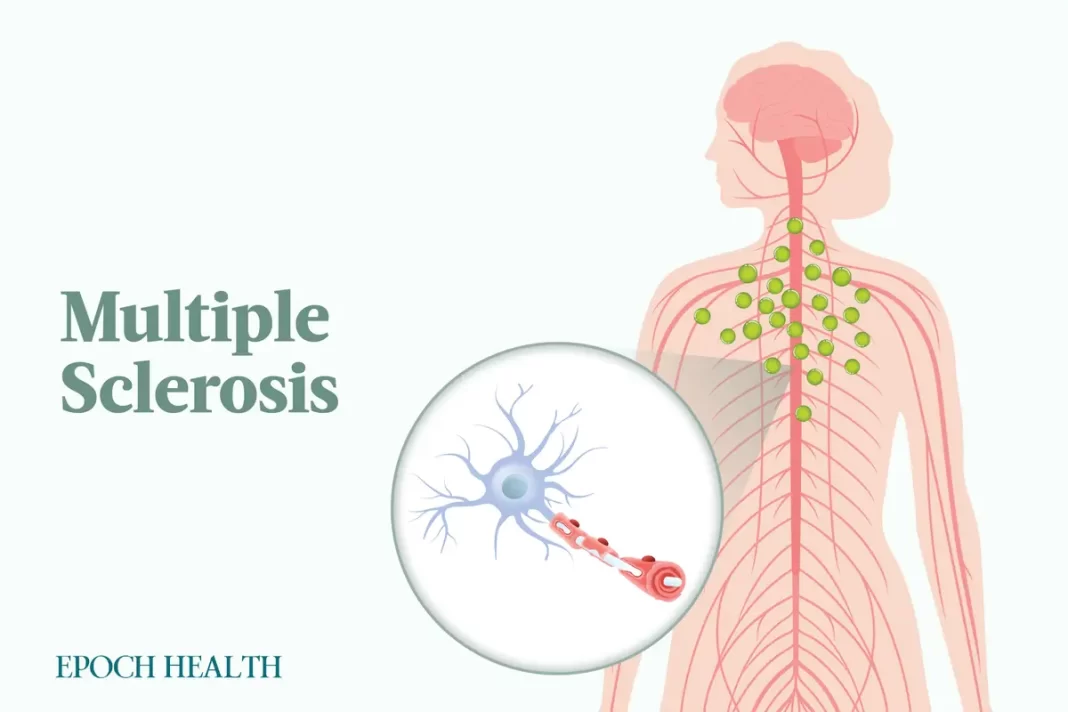
Multiple sclerosis (MS) is a chronic autoimmune condition affecting the central nervous system, including the brain and spinal cord. It occurs when the immune system mistakenly targets and harms the protective fatty myelin sheath surrounding nerves. Myelin plays a crucial role in insulating and safeguarding nerves, ensuring the electrical signals from the brain to the body travel swiftly and effectively. The disease can lead to issues with muscle coordination, vision, balance, sensation, and thinking, sometimes resulting in significant disabilities.
Typically, MS manifests between the ages of 20 and 40 and is the most common disabling neurological disease in young adults. Currently, nearly 1 million individuals in the United States are afflicted with MS.
What Are the Types of Multiple Sclerosis?
Different types of MS vary in their progression. Identifying a patient’s specific type of MS aids in anticipating its course and making informed treatment choices.
There are four types of multiple sclerosis, including the following:
1. Relapsing-Remitting Multiple Sclerosis (RRMS)
Relapsing-remitting MS is the most common form of MS, as it accounts for the initial diagnosis in around 85 percent of all MS cases. RRMS is marked by distinct episodes of active disease activity (i.e., attacks or relapses) followed by recovery (i.e., remission) phases.
Also known as “attacks” or “exacerbations,” MS relapses are abrupt, significantly worsening symptoms lasting at least 24 hours and not caused by infection, fever, or stress. They result from new areas of inflammation and demyelination. Demyelination is when the protective covering of nerve fibers, myelin, is damaged or destroyed. Most relapse symptoms improve with time, rest, and possibly therapy, but partial recovery can lead to permanent symptoms. MS relapses usually endure for days to weeks. People with RRMS not on disease-modifying therapy (DMT) typically have one to three relapses annually, but some experience much longer intervals between relapses.
In remission, the disease seems to halt its progression. During this phase, symptoms may not worsen or completely vanish (non-worsening), or some may worsen and become permanent (worsening).
Infection, fever, and stress can cause pseudo-relapses, which mimic real MS relapses but lack new inflammation or demyelination. Magnetic resonance imaging (MRI) scans aid in distinguishing between pseudo- and real relapses. Pseudo-relapses may be addressed by treating the underlying infection or stress source.
By Mercura Wang